
(Original article in English, auto-translated with Microsoft Translator in other languages)
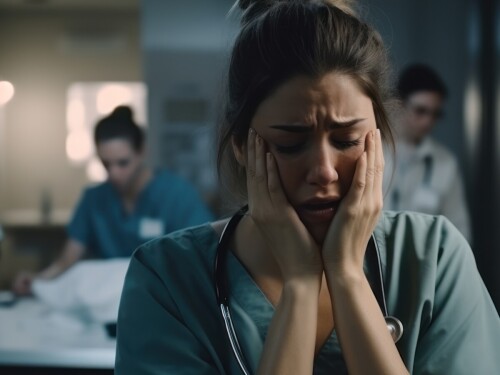
The demanding nature of the nursing profession, coupled with the high workload and long shifts, can take a toll on a nurse's well-being.[1] Nurses commitment to health care is essential, but this commitment often comes with an overlooked cost: nurse burnout.
The World Health Organization (WHO) defines burnout as a state of emotional, physical and mental exhaustion caused by exposure to chronic stressors in the workplace.[2] Nursing is an occupation that experiences one of the highest rates of burnout; the globally pooled prevalence of nurse burnout is 11.2%.[3] However, in other studies classifying burnout symptoms, nurse burnout was as high as 40.0%.[4] Moreover, nurse burnout in the post-COVID-19 pandemic era has worsened. In a recent study, nurse burnout was as high as 68.0%.[5] The impact of nurse burnout is significant in that it not only negatively influences nurses but also patients and healthcare organisations.[6]
Nurses must first know the signs of burnout in order to prevent it. Nursing burnout can surface in many ways (Table 1),[7] but it is frequently related to a handful of symptoms, like fatigue, dreading going to work, feeling underappreciated, and being constantly overworked. When these signs are ignored, burnout can lead to serious consequences, such as increased medical errors, decreased productivity, and a higher likelihood of leaving the nursing profession altogether.[8]
| Physical | Psychological | Emotional | Behavioural |
• Exhaustion | • Fatigue • Difficulty concentrating • Detached from staff and family • Decreased productivity • Decline in performance • Decreased creativity • Negative attitude • Decreased commitment • Loss of purpose • Anger, irritability • Increased anxiety | • Decreased personal accomplishment | • Calling in sick, arriving late, leaving early • Procrastinating • Withdrawn • Intolerance to change • Taking frustrations out on staff • Increased use of alcohol • Substance misuse • Social isolation |
To help maintain work-life balance and all-around wellness, nurses should establish good self-care habits that support their physical, mental and social health. Below are some practical strategies to help nurses take care of themselves amidst the demands of their profession. By implementing these tips, nurses can work towards creating a healthy work-life balance and nurture their physical, mental, and emotional health.
• Quality sleep is fundamental for cognitive function, emotional resilience, and physical well-being. Establish a consistent sleep schedule and create a conducive sleep environment.
• Nutrition plays a key role in maintaining energy levels and overall health. Focus on a well-balanced diet with a variety of nutrient-rich foods to support the body and mind.
• Physical activity is a powerful stress reducer. Integrate consistent physical activity into the daily schedule, whether through activities like walking, jogging, yoga, or any exercise that brings enjoyment
• Make time for activities outside of work that bring joy and relaxation. Engage in hobbies or leisure activities that provide a sense of fulfilment and balance.
• Recognise the importance of maintaining a healthy balance between work and personal life. Set clear boundaries regarding availability outside of work hours and communicate them effectively.
• Prioritise tasks and organise workloads. Learn to distinguish between urgent and important tasks, and delegate when appropriate to avoid becoming overwhelmed.
• Utilise breaks to relax and recharge. Step away from the workspace, engage in activities that bring joy, and avoid using breaks to catch up on work-related tasks.
• Prioritise lunch breaks as a time to nourish the body and mind. Step outside, if possible, connect with colleagues, or engage in activities that promote relaxation.
• Foster a supportive environment among colleagues. Share experiences, challenges, and successes to build a sense of camaraderie.
• Seek guidance from experienced nurses who can provide valuable insights and support professional development.
• Build a network of trusted friends and family members who can provide emotional support and understanding.
• Incorporate mindfulness into daily routines through practices such as deep breathing, meditation, or guided imagery. These techniques can help manage stress and enhance emotional well-being.
• Develop relaxation rituals before or after work, such as listening to calming music, taking a few minutes of quiet reflection, or engaging in a brief mindfulness exercise.
• Pursue ongoing education and professional development opportunities to stay motivated and engaged.
• Cultivate a mindset of continuous learning. Stay curious about advancements in the field and explore new areas of interest within healthcare.
• Acknowledge and celebrate both small and significant achievements. Regularly reflect on accomplishments to maintain a positive outlook.
• Set realistic goals for personal and professional growth. Break down larger goals into smaller, achievable steps to track progress.
• To proactively address the onset of burnout, it is beneficial to undertake a reflective exercise by cataloguing the specific stressors contributing to feelings of exhaustion. This involves attentively observing emotions and mood fluctuations during work, and identifying potential triggers.
• Take note of interactions with coworkers or patients, evaluate the impact of sleep deprivation, assess workloads. Developing a keen mental awareness of these stressors empowers you to pre-emptively recognise and navigate anxious situations, preventing them from significantly impacting emotional well-being.
• Recognise the importance of taking planned vacation days to rest and rejuvenate. Disconnect from work-related communication during time off.
• Acknowledge and process emotions related to patient care. Regular reflection can help prevent emotional exhaustion by providing an outlet for processing challenging situations.
• Consider seeking counselling or therapy to address emotional challenges and promote mental well-being.
1. Bean M. 31% of nurses cite burnout as reason for leaving job. https://www.beckershospitalreview.com/nursing/31-of-nurses-cite-burnout-as-reason-for-leaving-job.html
2. World Health Organization. Burn-out an "occupational phenomenon": International Classification of Diseases. 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
3. Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J Psychiatr Res. 2020;123:9–20.
4. Pradas-Hernández L, et al. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS ONE. 2018;13:e0195039.
5. Bruyneel A, Smith P, Tack J, Pirson M. Prevalence of burnout risk and factors associated with burnout risk among ICU nurses during the COVID-19 outbreak in French speaking Belgium. Intensive Crit Care Nurs. 2021;65:103059.
6. Nabizadeh-Gharghozar Z, Adib-Hajbaghery M, Bolandianbafghi S. Nurses' job burnout: A hybrid concept analysis. J Caring Sci. 2020;9:154–161.
7. Squellati R, Zangaro GA. Eight Ways Nurses Can Manage a Burnt-Out Leader. Nurs Clin North Am. 2022;57:67-78.
8. Portero de la Cruz Silvia, Cebrino Jesús, Herruzo Javier, et al. A multicenter study into burnout, perceived stress, job satisfaction, coping strategies, and general health among Emergency Department Nursing Staff. J Clin Med. 2020;9:1007.