
The treatment paradigm for multiple sclerosis (MS), particularly relapsing-remitting MS, is heavily reliant on biologic disease-modifying therapies (DMTs); however, the current cost of treatment can act as a significant barrier to access for many patients.1 Successor or ‘follow-on’ medicines may offer additional treatment options and savings for people with MS and include both generic medicines and biosimilars (Table 1). 2
A generic medication is created to be the same as a brand name medication, with the same dosage form, strength, quality and intended use.They are exact copies of medicines that are no longer patented.2,3

A biosimilar is a biologic medicine that is highly similar but not identical to its originator or reference product. It has no clinically meaningful differences compared with the reference product and therefore similar safety, efficacy and tolerability is anticipated.3
Biosimilar medicines approved in the EU are interchangeable with the reference medicine or equivalent biosimilar
Generic | Biosimilar |
| Usually produced by chemical synthesis | Obtained from a biological source |
Generally possible to obtain exactly the same molecule | Possible to reproduce the molecule to a high degree of similarity due to unique biomanufacturing methods and natural biological variability |
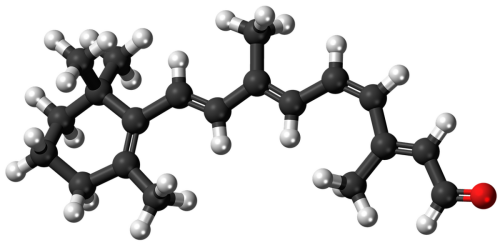
| Mostly smaller molecules, easier to characterise | In general, larger, structurally more complex molecules, which require multiple technologies for their characterisation |
| Full data requirements on pharmaceutical quality | Full data requirements on pharmaceutical quality, plus additional quality studies comparing the structure and biological activity of the biosimilar with the reference medicine |
| Development based on demonstration of bioequivalence (i.e. that the generic and the reference medicine release the active substance into the body at the same rate and to the same extent under similar conditions) | Development based on demonstration of biosimilarity using comparability studies (comprehensive head-to-head comparison of the biosimilar with the reference medicine to show high similarity in chemical structure, biological function, efficacy, safety and immunogenicity) |
| Clinical data requirements are mainly pharmacokinetic bioequivalence studies | In addition to comparative pharmacokinetic and pharmacodynamic studies, safety and efficacy data may be required, particularly for more complex biological medicines |
| All indications approved for the reference medicine can be granted based on demonstrated bioequivalence, without the need for further clinical data | Efficacy and safety have to be justified in each indication. However, confirmatory clinical trials with the biosimilar are usually not needed in every indication that has been approved for the reference medicine. After demonstration of biosimilarity, extrapolation of data to other indications is possible if the scientific evidence available addresses all specific aspects of these indications |
Biosimilar medicines can provide alternative treatment options to branded reference biologic medicines. They can offer advantages to EU healthcare systems, improving patients’ access to safe and effective biological medicines with proven quality. Branded biologic and biosimilar medicines are large, complex proteins, produced in living cells.
Biosimilars have the same amino acid sequence, route of administration and strength as their reference biologic. Table 2 shows the key properties of biologics versus biosimilars.

Biologicwith new active substance (reference medicine) | Biosimilar
|
| 15 years and $1.2 billion to develop | 8–10 years and $100–$200 million to develop |
| Patentable | Non-patentable |
No previous knowledge of safety and efficacy | Builds on knowledge of safety and efficacy from years of clinical use with reference medicine |
| Development aims at demonstrating safety and efficacy directly in patients | Development aims at demonstrating comparable safety and efficacy by establishing biosimilarity |
| Comparability studies only for manufacturing changes during development (e.g. producing larger batches for clinical trials) | Comprehensive comparability studies with the reference medicine |
| Full non-clinical data (pharmacology and toxicology) | Amount of non-clinical data determined by the outcome of quality studies |
| Conventional clinical trials to demonstrate efficacy and safety in all claimed therapeutic indications | Comparative clinical trials to exclude clinically meaningful differences |
| Trials designed mainly to compare with placebo or current standard of therapy using ‘hard’ endpoints (e.g. long-term outcome, mortality, structural damage) and a relevant patient population to demonstrate benefit | Trials designed mainly to show clinical equivalence with the reference medicine using sensitive endpoints in a population where product-related differences in clinical performance can be detected |
| Positive benefit-risk mainly established on the basis of safety and efficacy studies in the intended population | Positive benefit-risk based on demonstrating biosimilarity (using comparability studies) |
Generic non-biological complex drugs (e.g. glatiramer acetate) and generic small molecules (e.g. dimethyl fumarate; fingolimod; teriflunomide) have already been approved for MS in Europe.2 Generic medications are also often prescribed to help manage symptoms of MS, for example baclofen, pregabalin and sildenafil citrate.6,7

Tyruko® (natalizumab) is the first and currently only available biosimilar available for MS in Europe.8 In September 2023, the European Commission approved Tyruko® for the treatment of adults with highly active relapsing-remitting MS. The biosimilar was originally developed by Polpharma Biologics and is now marketed by Sandoz.
The approval was based on results from a Phase I pharmacokinetic/pharmacodynamic study and a confirmatory Phase III Antelope study in people with relapsing-remitting MS.9
Both studies met their primary endpoints, confirming that the biosimilar matches the reference biologic in terms of pharmacokinetics as well as efficacy, safety and immunogenicity. Tyruko® has the same strength/ dosage form, intravenous (IV) route of administration, dosing regimen and presentation as the reference medicine. The study also included a subgroup of patients who switched over from the reference natalizumab to the biosimilar and there were no significant differences observed in terms of safety, tolerability or immunogenicity.
As biosimilars begin to become available, it is important for the MS Nurse to ensure they are fully educated regarding the options, so that they are able to communicate effectively with the PwMS.
Studies in other therapy areas, where biosimilars are more established, have shown that the relationship between the healthcare provider and the patient is the foundation of how people will perceive and accept the new biosimilar treatments, limiting the risk of negative bias and the nocebo effect.10
This refers to the negative effects that result from the anticipation or expectation of harm, often leading to the worsening of symptoms or outcomes. It is common among neurological patients and affects adherence and treatment outcomes, representing a real clinical challenge.11
Nocebo risk can be minimised with education – closing the knowledge gap about generics and biosimilar medicines – to aid healthcare provider and patient understanding and confidence in the value of a medicine.11

In a recent set of consensus recommendations, Use of Follow-on Disease Modifying Treatments for Multiple Sclerosis, important points that should be considered include:
Making sure people have all the information they need to understand the difference between reference and biosimilar products is an essential task for the MS Nurse and might include:
Following any switch, it is important that the MS nurse sees the PwMS on a regular basis.
This might take the form of a patient support programme (face-to-face, online or via Apps) to re-inform the person, to ensure adherence and/or manage side-effects.
It is important for MS Nurses to have a good understanding of generics and biosimilars, including what they are and how they are approved by regulatory agencies, and to have confidence in discussing these with PwMS as they are likely to become an increasing part of clinical practice moving forward.
1. MS International Federation. Atlas of MS 3rd edition: Clinical management of multiple sclerosis around the world. Available from: https://www.msif.org/wp-content/uploads/2021/05/Atlas-3rd-Edition-clinical-management-report-EN-5-5-21.pdf. [Accessed August 2024]
2. Greenberg B, Giovannoni G. A place for biosimilars in the changing multiple sclerosis treatment landscape. Mult Scler Relat Disord. 2023;77:104841
3. European Medicines Agency and the European Commission. Biosimilars in the EU: Information guide for healthcare professionals. Updated November 2023. [Accessed August 2024].
Available at: https://www.ema.europa.eu/en/documents/leaflet/biosimilars-eu-information-guide-healthcare-professionals_en.pdf . [Accessed August 2024]
4.EMA. Biosimilar medicines can be interchanged. 2022.
Available at: https://www.ema.europa.eu/en/news/biosimilar-medicines-can-be-interchanged . Accessed August 2024.
5.US Food and Drug Administration. Biosimilars. Available at: https://www.fda.gov/drugs/therapeutic-biologics-applications-bla/biosimilars . Accessed August 2024.
6. Generic and biosimilar medications. National MS Society.
Available at: https://www.nationalmssociety.org/managing-ms/treating-ms/disease-modifying-therapies/generic-biosimilars . [Accessed August 2024]
7.MS Trust. Generic and biosimilar drugs in MS. Available at: https://mstrust.org.uk/a-z/generic-and-biosimilar-drugs-ms . [Accessed August 2024]
8. Novartis Pharma AG. https://www.globenewswire.com/news-release/2023/09/26/2749144/0/en/Sandoz-receives-European-Commission-approval-for-Tyruko-natalizumab-first-and-only-biosimilar-for-multiple-sclerosis-in-Europe.html . [Accessed August 2024]
9.Hemmer B, et al. Efficacy and Safety of Proposed Biosimilar Natalizumab (PB006) in Patients With Relapsing-Remitting Multiple Sclerosis: The Antelope Phase 3 Randomized Clinical Trial. JAMA Neurol. 2023;80(3):298-307
10. Pouillon L, et al. Consensus report: clinical recommendations for the prevention and management of the nocebo effect in biosimilar-treated IBD patients. Aliment Pharmacol Ther. 2019;49:1181-1187.
11. Spanou I, et al. Nocebo in biosimilars and generics in neurology: a systematic review. Front Pharmacol. 2019; 10:809.
12. Brownlee WJ, et al. Use of Follow-on Disease Modifying Treatments for Multiple Sclerosis: Consensus recommendations. Mult Scler. 2022;28:2177-2189.
All Blogposts, e-learning Courses, e-Newsletters, e-Newsflashes and the website content of MS Nurse PRO is originally created in English (UK).
Our Educational Read Blogposts and our e-learning courses are reviewed by our scientific committee on accuracy and objectiveness.
Next, the content is auto-translated by Microsoft Translator and made available on our platform.
The translated content is not language reviewed with the exception of our e-learning Course content.
MS Nurse PRO has put a process in place to have our e-learning Courses language reviewed by native speaking experts (nurses or neurologists). We make all translated e-learning Courses available immediately and next, the language review process is started. This review process can take several months.